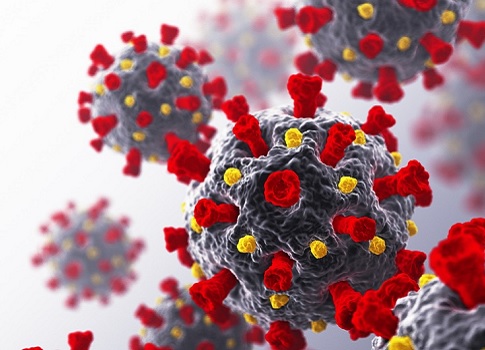
COVID-19
/ˈkō-vid-nīn-ˈtēn/ (noun)
a mild to severe respiratory illness that is caused by a coronavirus (Severe acute respiratory syndrome coronavirus 2 of the genus Betacoronavirus); is transmitted chiefly by contact with infectious material (such as respiratory droplets) or with objects or surfaces contaminated by the causative virus; and is characterized especially by fever, cough, and shortness of breath and may progress to pneumonia and respiratory failure
We’ve curated this collection of resources to help you help your patients, staff and their families to navigate, manage and treat the virus.
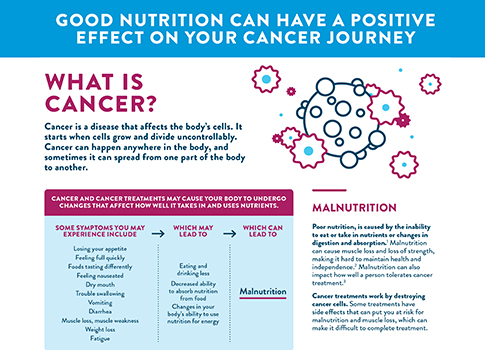
CANCER
/kansər (noun)
a malignant growth or tumor resulting from the division of abnormal cells.
According to the National Cancer Institute, cancer is the name given to a collection of related diseases. In all types of cancer, some of the body’s cells begin to divide without stopping and spread into surrounding tissues.
We’ve curated this collection of education and nutrition-related resources to help you support your patients during their cancer journey.
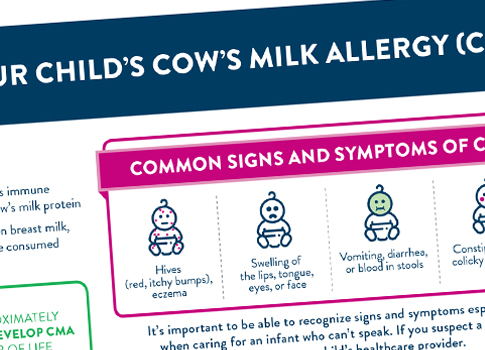
FOOD ALLERGIES
/ˌfo͞odˈalərjē/
(noun)
a damaging immune response by the body to a particular food, to which it has become hypersensitive
According to Food Allergy Research & Education (FARE), “32 million Americans have food allergies, including 5.6 million children under age 18. That’s one in 13 children, or roughly two in every classroom…[and] about 40 percent of children with food allergies are allergic to more than one food.” We’ve curated this collection of resources to help you help your pediatric patients and their families to navigate and manage food allergies.
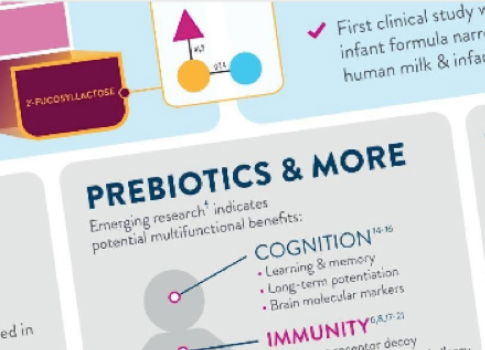
Human Milk Oligosaccharides
/, (h)yo͞omən/ milk/ ˌäləɡōˈsakəˌrīds/ (noun) a family of structurally diverse unconjugated glycans that are found in, and unique to, human breast milk.
Recent studies show that 2’-FL HMO—a prebiotic found naturally in human milk—can serve as food for beneficial bacteria in the infant gut. Learn more about how HMOs expand beyond the gut to support the immune system.
Malnutrition
/ˌmaln(y)o͞oˈtriSH(ə)n/ (noun) lack of proper nutrition, caused by not having enough to eat, not eating enough of the right things, or being unable to use the food available
The World Health Organization reports that one-third of the global population suffers from malnutrition complications, like stunting, wasting, obesity, vitamin and mineral deficiency, and some non-communicable diseases. Learn what you can do to reduce the burden of malnutrition in the communities you serve.

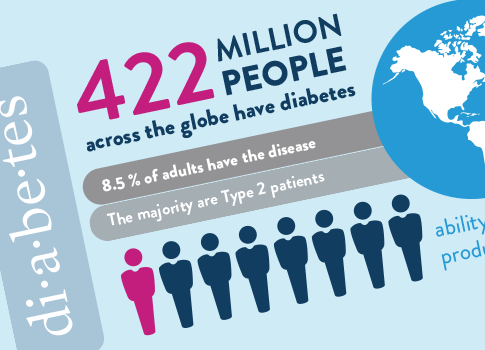
Diabetes
/ˌdīəˈbēdēz,ˌdīəˈbēdis/ (noun) a disease in which the body’s ability to produce or respond to the hormone insulin is impaired, resulting in abnormal metabolism of carbohydrates and elevated levels of glucose in the blood and urine.
According to the World Health Organization, 422 million people across the globe have diabetes; 8.5% of all adults live with diabetes, and the majority are patients with Type 2 diabetes. Learn more about the role nutrition can play in better patient outcomes.
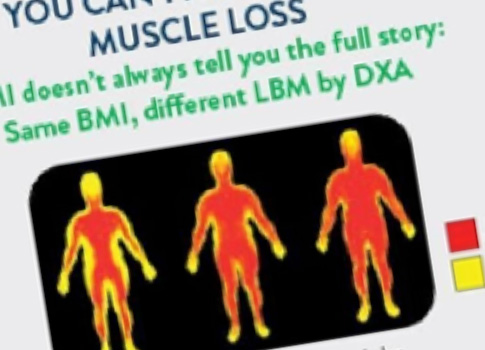
Muscle Mass
/lēn/ /ˈbädē/ /mas/ (noun) the total weight of your body minus all the weight due to your fat mass; it includes the weight of all your organs, skin, bones, body water, and muscles.
Many patients are at risk for muscle loss, especially those with advancing age or acute and chronic conditions. And, often, a person’s muscle mass plays a role in their quality of life, recovery, and physical function. Learn how to help your patients maintain muscle mass for better outcomes.